Nephrotic Syndrome and diuretic, its types and mechanism:
THE NEPHROTIC SYNDROME
It is a condition characterised by loss of Large quantities of plasma proteins into the urine. Is caused by increased permeability of the glomerular membrane.
Conditions leading to NS
- Chronic glomerulonephritis.
- Amyloidosis, which results from the deposit, ion of an abnormal proteinoid substance in the walls of the blood vessels and seriously damages the basement membrane of the glomerulus.
- Minimal change disease Found mainly in young children.
“Minimal Change Nephrotic Syndrome
In this disease, the negative electrical charge normally exhibited by the glomerular membrane is reduced or lacking.As a result loss of the negative charge allows proteins, especially albumin, to pass through the glomerular membrane with ease.
This disease occurs mainly in children between the ages of 2 and 6 years.This condition leads. To very severe low protein edema. Approximately 90 percent of these children respond exceedingly well to the administration of glucocorticoid steroids.
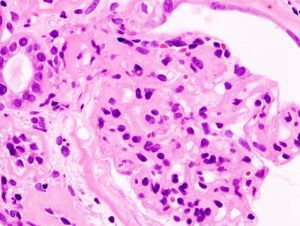
Histopathological image of diabetic glomerulosclerosis with nephrotic syndrome
SPECIFIC TUBULAR DISORDERS
1 Renal Glycosuria this condition the blood glucose concentration may be completely normal, reabsorption but the transport more absorption of glucose is greatly limited or absent. As a result large quantities of glucose pass into the urine each day.
- Excess Proximal Tubular
Reabsorption of Urate lon (The Cause of Gout)
The renal tubules have the capability of both actively secreting urate ions and actively reabsorbing it. The active reabsorption proceri occurs in the proximal tubules. In a small subsat of persons this reabsorption is overly active and causes persistently elevated urate ions in the extracellular fluid.
Above a critical concentration, urate precipitates in many tissues of the body in the form of uric acid crystals. Precipitation occurs especially in the joints, leading to the clinical syndrome known as “gout” a type of inflammatory arthritis that can effect multiple joints at a time.
- Nephrogenic Diabetes Insipidus
In this renal tubules do not respond to antidiuretic hormone secreted by the supraopticohypophyseal system; as a consequence, large quantites of dilute urine are continually excreted.
- Renal hypophoshatemia this condition renal tubules fail to reabsorb adequate quantities of phosphate ions even when the phosphate concentration of the body fluids falls very low.
- Aminoaciduria
- Generalized aminoaciduria : deficient reabsorption of all amino acids.
- Essential, cystinuria : large amounts of cystine fail to be reabsorbed and often eystalize in the urine to form renal stones.
- Simple glycinuria glycine fails to be reabsorbed.
- Beta amino-isobutyric aciduria
has little or no clinical significance.
RENAL FUNCTION TESTS
Three main categories are there:
- Determination of renal clearance.
- Measurement of substances in the blood that are normally excreted by the kidneys.
- Chemical and physical analysis of the urine, Volume of urine, Specific gravity, Colour, Smell.
DIURETICS AND MECHANISMS OF THEIR ACTIONS
A diuretic is a substance that increases the rate of urine output.
Most diuretics act by decreasing the rate of reaborption of fluid from the tubule. Principle use of diuretics is to reduce the total amount of fluid in the body. They are especially important. In treating edema and hypertension. when a diuretic is used, it is important to note that the rate of sodium loss in the urine will also be increased as well as the rate of water loss.
TYPES OF DIURETICS
- The Osmotic Diuretics
Examples are urea, sucrose, mannitol, the osmotic pressure of these greatly decreases water reabsorption, so that large amounts of tubular fluid flush into the urine.
- The diuretics that decrease active reabsorption are
a.The Loop Diuretics e.g. Furosemide and Ethacrynic Acid.
b.Chlorothiazide,
c.Carbonic Anhydrase Inhibitors I.e. Acetazolamide.
d.Competitive A1dosterone Inhibitors i.e. spironolactone.
Leave a Reply